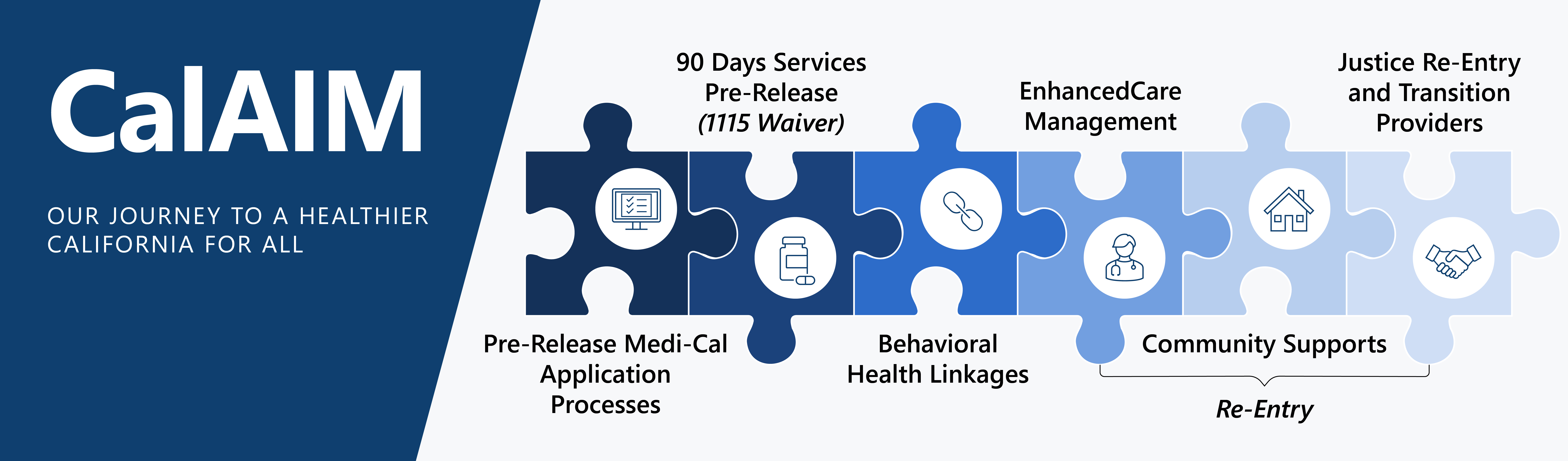
CDCR/CCHCS will break ground by becoming the first prison system in the U.S. to become a state-sponsored health coverage billing entity. Becoming a Medi-Cal billing entity will allow CDCR/CCHCS to receive reimbursements for a limited set of 90-day pre-release services, including medications, durable medical equipment, expanded pre-release planning and enhanced care management coordination. This initiative is part of California Advancing and Innovating Medi-Cal (CalAIM), a multiyear reform led by the California Department of Health Care Services (DHCS) to improve the health outcomes and overall well-being of Medi-Cal enrollees. Based on Quality Management (QM) projections and CalAIM eligibility criteria, about 73% of the CDCR population, or about 69,000 people will be CalAIM eligible. This means the participants will first be Medi-Cal eligible (with Medi-Cal benefits activated 90 days prior to release). Thereafter, those with a mental health, medical or substance use disorder treatment need will be CalAIM Access eligible.
Timeline
- DHCS is requiring CDCR/CCHCS to become a fully billable and claiming entity no later than March 31, 2026.
- CDCR/CCHCS currently provide Medi-Cal benefit application assistance through the Transitional Case Management Program (TCMP). CalAIM will require counties to activate those benefits 90 days prior to release.
- CDCR/CCHCS will begin CalAIM 90-day pre-release services immediately upon the Medi-Cal Reimbursement System (MCRS) technology solution going live.
Goals
- Enhance Medi-Cal Application Process
- Identify enhancements to the current Medi-Cal application process and identify automation application and eligibility processes between 58 counties, 33 prisons, and HQ.
- Applications will be submitted 135 days prior to release. Application status will be updated no later than 90 days before release.
- 90-day Pre-Release Eligibility Screening
- Automate Medi-Cal and Medical Systems to flag participants who are CalAIM eligible.
- Automate notifications to state eligibility systems for release date and CalAIM eligibility.
- 90-day Pre-Release Services
- Develop a system to bill Magellan for medication reimbursements.
- Develop a system to bill CA-MMIS for reimbursement of pre-release services and durable medical equipment.
- Reentry Plan Planning and Coordination
- Develop a system to bill CA-MMIS for reimbursement of reentry planning, enhanced care management coordination, and warm handoffs.
Milestones
- DHCS to finalize policy guidelines in October 2023.
- CDCR/CCHCS review final requirements, continue workgroups to create new Care Coordination workflows including billing protocols.
- IT to continue to build MCRS (to submit claims and provide intelligent workflows).
- Five months prior to Go-Live, CDCR/CCHCS enrolls as a Medi-Cal Provider.
- Institutions to enroll as Exempt from Licensure option, allowing providers to fall under a main National Provider Identifier.
- All CDCR/CCHCS pharmacies will enroll individually.
- DHCS committed to working with CDCR/CCHCS through the enrollment process.
- Five months prior to Go-Live, CDCR/CCHCS works with DHCS to submit DHCS Readiness Assessment.

